Treatment
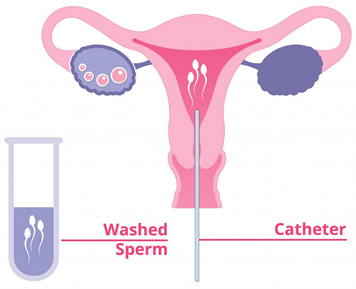
I) IUI (Intrauterine Insemination) along with Superovulation
- Intrauterine insemination (IUI) is a fertility treatment that involves placing sperm inside a woman’s uterus to facilitate fertilization. The goal of IUI is to increase the number of sperm that reach the fallopian tubes and subsequently increase the chance of fertilization. IUI provides the sperm an advantage by giving it a head start, but still requires a sperm to reach and fertilize the egg on its own. It is a less invasive and less expensive option compared to in vitro fertilization. The most common reasons for IUI are a low sperm count or decreased sperm mobility.
- However, IUI may be selected as a fertility treatment for any of the following conditions as well:
- Unexplained infertility
- A hostile cervical condition, including cervical mucus problems
- Cervical scar tissue from past procedures which may hinder the sperms’ ability to enter the uterus
- Ejaculation dysfunction
- IUI is not recommended for the following patients:
- Women who have severe disease of the fallopian tubes
- Women with a history of pelvic infections
- Women with moderate to severe endometriosis
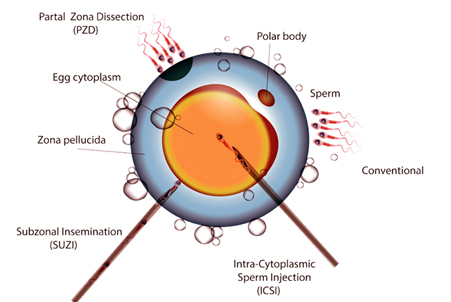
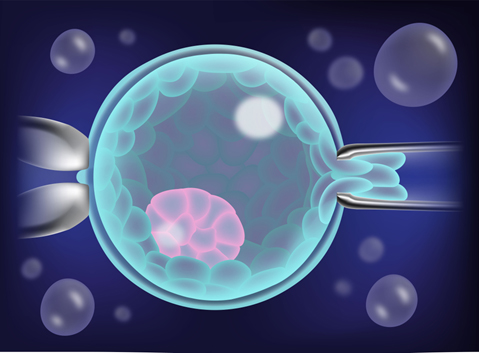
II) ICSI (Intracytoplasmic Sperm Injection)
- Intracytoplasmic sperm injection process takes place during IVF. It is often performed for couples that are dealing with male factor infertility and for those who have not had success with IVF in the past.
- There are five main steps to the ICSI procedure:
- A sperm sample is taken from your partner’s semen or surgically extracted from his testes or epididymis.
- Your eggs are surgically extracted from your ovaries.
- Using a tiny hollow needle, one sperm is carefully injected into an egg.
- After injection, the fertilized egg is observed for growth and development.
- Once normal growth is observed, the embryo will be implanted into your uterus where it has a chance to implant and grow.
- Some fertility clinics choose to use fresh sperm that have just been extracted, while others prefer to do the ICSI procedure with frozen sperm. There appears to be no difference in pregnancy rates between those who use fresh or frozen sperm during the ICSI process.
- How ICSI works
- The ICSI procedure is performed by using a technique called micromanipulation. Micromanipulation uses a special microscope, along with very small surgical tools, to pick up and handle one single sperm, injecting it directly into an egg. ICSI and male infertility The ICSI procedure can help you achieve IVF pregnancy success even when male infertility problems are an issue.
III) IVF (In Vitro fertilization)
- IVF or In Vitro Fertilization is an assisted reproductive technology (ART) commonly referred to as IVF. IVF is the process of fertilization by extracting eggs, retrieving a sperm sample, and then manually combining an egg and sperm in a laboratory dish. The embryo(s) is then transferred to the uterus. Other forms of ART include gamete intrafallopian transfer (GIFT) and zygote intrafallopian transfer (ZIFT).
- Why is IVF used?
- IVF can be used to treat infertility in the following patients: Blocked or damaged fallopian tubes
- Male factor infertility including decreased sperm count or sperm motility
- Women with ovulation disorders, premature ovarian failure, uterine fibroids
- Women who have had their fallopian tubes removed
- Individuals with a genetic disorder
- Unexplained infertility
- The IVF process involves:
- Stimulating multiple follicles and eggs to develop Egg retrieval to get the eggs Fertilizing the eggs in the laboratory, Embryo transfer to the uterus
- Louise Brown was the first IVF baby in the world. She was born in July of 1978 in England by IVF procedure. Louise was 28 (in 2006) when she had her own baby (without IVF).
- Hundreds of thousands of children are now born every year as a result of IVF .
IV) Surgical Sperm Retrieval (PESA/TESA/TESE/MESA)
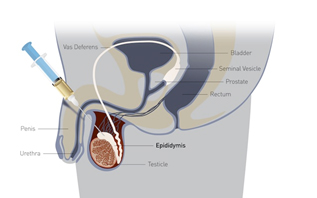
- PESA
PESA (percutaneous epididymal sperm aspiration) is a method, performed under local anesthesia, which involves extracting sperm with a fine needle from the epididymis or testes. The sperm is then implanted into the egg through the process of ICSI (Intracytoplasmic Sperm Injection) to be used in IVF.
- TESA & TESE
In cases where the epididymis does not contain any sperm, because of impaired sperm production, the method of TESA (Testicular Sperm Aspiration) or TESE (Testicular Sperm Extraction) may be used. TESE involves a surgical biopsy of the testis, while TESA is performed by sticking a needle into the testis and aspirating fluid and tissue with negative pressure.
- MESA
The most invasive of the surgical sperm retrieval procedures is MESA (micro-epididymal sperm aspiration), which is performed under general anesthesia. MESA involves the cutting open of the scrotum to retrieve sperm. The wound is closed with dissolvable stitches. Swelling and pain subsides within a few days, during which prescribed painkillers may be taken to ease the pain. These alternative methods of retrieving sperm allow male patients to use their own sperm in the IVF procedure. The procedures themselves are not very costly and offer the chance for couples to avoid the cost of using a sperm donor. At the Cyprus Fertility Clinic, we are committed to offering you low cost IVF treatment with high success rates. Some men do not produce sperm at all or only in insufficient numbers and poor quality. Many of these men can have their sperm aspirated directly from their testicles (TESA) or from the epididymis that stores the sperm prior to an ejaculation (PESA, MESA). The retrieved sperm are then used during in vitro fertilization, gestational surrogacy or egg donation treatments with Intracytoplasmic Sperm Injection (ICSI). The aspiration is a brief outpatient procedure requiring only mild sedation. Most sperm aspiration procedures are performed at our centre.
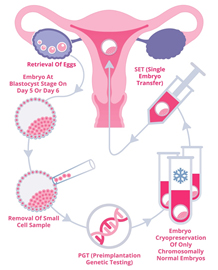
V) PREIMPLANTATION GENETIC DIAGNOSIS (PGD)
- Preimplantation genetic diagnosis (PGD) is a reproductive technology used with an IVF cycle. PGD can be used for diagnosis of a genetic disease in early embryos prior to implantation and pregnancy. All we can do is eliminate heartbreaking and devastating genetic diseases caused by mutations in either or both husband and wife. This genetic testing could be used for sex selection, but we do not believe that this is legitimate, and will not do it even though we easily could.
- There are two different kinds of PGD, either to eliminate parental mutations or to test for chromosomal number (aneuploidy screening). The later is used widely, but is usually more harmful than beneficial, for fascinating reasons, that I will explain later. The former, eliminating mutations of carriers of genetic disease is extremely effective and beneficial.
- WHAT IS EMBRYO BIOPSY?
When an embryo reaches the third day of development, it normally has eight cells. One or two of these cells, called “blastomeres”, can be removed from the embryo with micromanipulation technique. The embryo is usually unharmed, and can go on to develop just as though this one cell were never removed. Of course it is not always true that there is no harm. The same can be done with the trophoblast of day 5 embryos. You can then subject those cells to genetic analysis, and know the chromosomal composition of the embryos, and if they carry a specific disease-producing mutation. Ironically it lowers the pregnancy rate. But it is a big money maker, and often is used inappropriately.
VI) Blastocyst Transfer
- What Is A Blastocyst?
During conception inside a woman’s body, the egg is fertilized by sperm in the fallopian tube and an embryo is formed. Eggs are retrieved from a woman’s ovaries, fertilized with sperm, and an embryo is created. The embryo divides and multiplies its cells over 5 to 6 days to become a blastocyst. Embryos that survive to this stage of development have a high implantation potential once transferred into the uterine cavity.
- Grade 1:
The embryo has the appropriate cell number for stage of development (eg., on day three, embryos should have 8 cells, also known as blastomeres) and the cells are even in their size and shape. The embryos should have little or no fragmentation (small amounts of extracellular debris) between cells.
- Grade 2:
The embryo has the correct development of cell numbers (6-8 cells on day three), with a small amount of fragmentation (20% fragmentation), or slight uneveness of blastomere sizes. grade 3 the embryo contains blastomeres that are uneven in size and has more than 30% fragmentation. embryos developing slowly will also receive a grade of 2 or 3 even if they are normal otherwise. grade 4 the embryo contains very few, if any, viable appearing cells and has a high percent fragmentation (over 50%).

VII) Infertility Work up
- Practice Essentials:
Infertility is the failure to conceive (regardless of cause) after 1 year of unprotected intercourse. This condition affects approximately 10-15% of reproductive-aged couples.
- Female factors that affect fertility include the following categories:
- Cervical: Stenosis or abnormalities of the mucus-sperm interaction
- Uterine: Congenital or acquired defects; may affect endometrium or myometrium; may be associated with primary infertility or with pregnancy wastage and premature delivery
- Ovarian: Alteration in the frequency and duration of the menstrual cycle—Failure to ovulate is the most common infertility problem
- Tubal: Abnormalities or damage to the fallopian tube; may be congenital or acquired
- Peritoneal: Anatomic defects or physiologic dysfunctions (eg, infection, adhesions, adnexal masses)
- Male factors that affect fertility include the following categories:
- Pre testicular: Congenital or acquired diseases of the hypothalamus, pituitary, or peripheral organs that alter the hypothalamic-pituitary axis
- Testicular: Genetic or non genetic
- Post testicular: Congenital or acquired factors that disrupt normal transport of sperm through the ductal system
- Treatment of infertility
- Treatment plans are based on the diagnosis, duration of infertility, and the woman’s age. Management of any underlying female and/or male factors affecting fertility may include medical treatment (e g, pharmacotherapy), surgical intervention, or both.

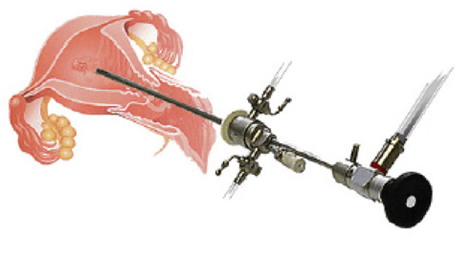
VIII) Hysteroscopy
- Hysteroscopy is a procedure that allows your doctor to look inside your uterus in order to diagnose and treat causes of abnormal bleeding. Hysteroscopy is done using a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus. Hysteroscopy can be either diagnostic or operative. Prior to the procedure, your doctor may prescribe a sedative to help you relax. You will then be prepared for anesthesia.
- The procedure itself takes place in the following order:
- The doctor will dilate (widen) your cervix to allow the hysteroscope to be inserted.
- The hysteroscope is inserted through your vagina and cervix into the uterus.
- Carbon dioxide gas or a liquid solution is then inserted into the uterus, through the hysteroscope, to expand it and to clear away any blood or mucus.
- Next, a light shone through the hysteroscope allows your doctor to see your uterus and the openings of the fallopian tubes into the uterine cavity.
- Finally, if surgery needs to be performed, small instruments are inserted into the uterus through the hysteroscope.
- The time it takes to perform hysteroscopy can range from less than 5 minutes to more than an hour. The length of the procedure depends on whether it is diagnostic or operative and whether an additional procedure, such as laparoscopy, is done at the same time. In general, however, diagnostic hysteroscopy takes less time than operative.
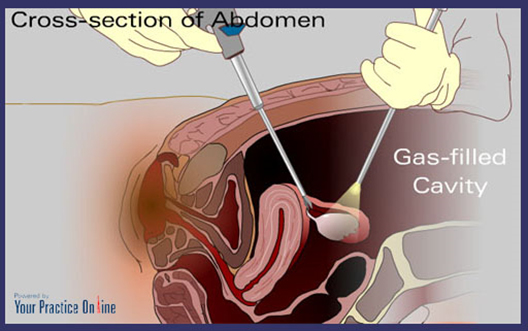
IX) Laproscopic diagnosis and Surgery
- Laparoscopy, also known as diagnostic laparoscopy, is a surgical diagnostic procedure used to examine the organs inside the abdomen. It is a low-risk, minimally invasive procedure. Only small incisions are made.
- Laparoscopy uses an instrument called a laparoscope to look at the abdominal organs. A laparoscope is a long, thin tube with a high-intensity light and a high-resolution camera at the front.
- The instrument is inserted through an incision in the abdominal wall. As it moves along, the camera sends images to a video monitor. Laparoscopy allows your doctor to see inside your body in real time, without open surgery. Your doctor also can obtain biopsy samples during this procedure.
- Why Is Laparoscopy Performed?
- Laparoscopy is often used to identify and diagnose the source of abdominal or pelvic pain. It’s usually performed when other, noninvasive methods are unable to help with diagnosis.
In many cases, abdominal problems can also be diagnosed with imaging techniques such as: - Ultrasound, which uses high-frequency sound waves to create images of the body
- CT scan, which is a series of special X-rays that take cross-sectional images of the body
- MRI, which uses magnets and radio waves to produce images of the body
- Laparoscopy is performed when these tests don’t provide enough information or insight for a diagnosis. The procedure may also be used to take a biopsy, or sample of tissue, from a particular organ in the abdomen.
X) Cyropreservation of Sperms /Egg or Embryos (Also known as Egg, Embyo and Sperm freezing)
Short-term semen cryobanking is the depositing, freezing and storage of sperm at a sperm bank for less than one year. Cryobanked sperm is then used in artificial insemination, in vitro fertilization (IVF) and other fertility treatment procedures.
- Long-Term Semen Cryopreservation
Proven, time-tested techniques enable semen specimens and embryos to be frozen and stored indefinitely in liquid nitrogen. According to the donor’s specific wishes, these specimens and embryos can later be thawed and used in an attempt to conceive through artificial insemination, IVF or other fertility treatment techniques.
- Cryopreservation Technique and Identification
Each sample (ejaculate) is mixed with a special media or solution to help provide protection during freezing and thawing. The samples are then placed in special plastic vials, which are coded, and carefully frozen in liquid nitrogen vapor. Once frozen, the vials are immersed in liquid nitrogen in secure tanks at a temperature of -196° C (-371° F). The liquid nitrogen is independent of any source of power, and is regularly checked and replenished. Each patient is assigned a unique “cryo code” and the sperm sample is processed individually using permanently marked vials by our licensed and certified clinical lab scientists.
- Embryo cryopreservation is useful ,if after a cycle of in vitro fertilisation, as patients who fail to conceive may become pregnant using such embryos without having to go through a full IVF cycle

XI) Laser Assisted Hatching
- What Is Assisted Hatching?
- After an egg is fertilized in the laboratory, the cells begin to divide. During these initial stages of development, the embryo is contained in a layer of proteins known as the zona pellicuda. In order to successfully implant into the uterine lining, an embryo has to hatch out of the zona pellucida and attach to the walls of the uterus.
- Assisted hatching is a newer lab technique that was developed when fertility experts observed that embryos with a thin zona pellucida had a higher rate of implantation during IVF. With assisted hatching, an embryologist uses micromanipulation under a microscope to create a small hole in the zona pellucida. This happens on the fourth day of embryo development when the embryos contain an average of six to eight cells. The embryos are stabilized by a holding pipette, and on the opposite side a small pipette containing an acidified solution creates a small defect in the zona pellucida. The embryos are then rinsed to remove any excess acid solution and returned to the incubator for a few hours before transfer into the uterus.
- Who Should Use Assisted Hatching with IVF?
- Assisted hatching is thought to be helpful for couples with a poor prognosis whose embryos are thought to lack sufficient energy to complete the hatching process. According to the American Society for Reproductive Medicine, assisted hatching may be indicated for women with:
- Advanced maternal age (older than 38)
- Two or more failed IVF cycles
- Poor embryo quality

XII) Surrogacy (Gestational Carrier)
Surrogacy is an arrangement, supported by a legal agreement, whereby a woman (the surrogate mother) agrees to bear a child for another person or persons, who will become the child’s parent(s) after birth. As per GOI Surrogate should be relative to the couple
XIII) Recurrent Pregnancy Loss
- Recurrent pregnancy lossis classically defined as the occurrence of two or more consecutive pregnancy loss, clinically-recognized pregnancy involuntarily ending before 20 weeks. A clinically-recognized pregnancy means that the pregnancy has been visualized on an ultrasound or that pregnancy tissue was identified after a pregnancy loss.
- The treatment recommendations for patients with recurrent pregnancy loss are based on the underlying cause of recurrent pregnancy loss.
- In our centre we provide state of art treatment for recurrent pregnancy loss with tender loving care.
There are lots of causes for recurrent pregnancy loss to be discussed medically , so we have to individualize the treatment
XIV) Stem Cell Therapy
- Stem cell therapy in India is emerging as a new modality within the healthcare system.
- We along with Ree Labs, a leading stem cell bank in India that is supporting the collection & offer stem cell treatment for various chronic, degenerative diseases, including Autism, Cerebral Palsy, Chronic Kidney Diseases, Chronic Liver Diseases, Cardiovascular diseases, Diabetes Type 1 and 2, ALS, Multiple Sclerosis, Spinal cord injury, stroke, Muscular Dystrophy, Parkinson’s disease, Alzheimer’s disease, Macular Degeneration, Retinitis Pigmentosa, Osteoarthritis, Hair-loss and Anti-aging etc.
XV) Other Services
- IVF Facilities are:-
- Tubal microsurgery
- Fertility enhancing laparoscopic & hysteroscopic surgeries
- Surgery for male infertility
- Hormonal manipulations
- Medical management of male infertility
- Intrauterine Insemination (husband/donor)
- IVF-ET (In vitro fertilisation- Test tube baby)
- ICSI (Intra cytoplasmic sperm injection- micromanipulation)
- Donor Oocyte IVF
- Embryo Donation
- Delivery
- LSCS
- MTP
- D&C
- All types of Hysterectomies
- Other Gynae & Obstretical Services


